by Joshua Dubin, DC, CCSP, CSCS, Rachel Dubin, DPT, Gregory Doerr, DC, CCSP
ABSTRACT:
Shin splints is an injury of the lower leg that often afflicts athletes. Generally, symptoms include pain on the anterolateral or posteromedial surfaces of the shin. There is a great deal of research on the treatment and prevention of shin splints, and based on extensive research, several hypotheses have been proposed for its pathophysiology; however, the exact cause of shin splints remains unknown. This paper explains the anatomy of the lower leg and biomechanics of gait. It presents possible etiologies and risk factors for shin splints, and it reviews options for treatment and prevention. Its conclusion, based on extensive literature review, reveals that most cases of shin splints respond favorably to conservative care. Such care generally includes home exercise, training and equipment modifications, and treatment by a skilled practitioner. However, in more advanced cases surgery may be necessary.
Introduction and History:
Shin splints is one of the most common exercise induced lower extremity injuries in athletes participating in activities that require prolonged or quick bursts of running and/or jumping.1 Such activities may include track and field, soccer, basketball, volleyball, basic military training, and long-distance running.7-11
During running each foot strikes the ground approximately 50-70 times per minute, or a total of 800 times per mile, with a force 2-4 times body weight.1,12 The muscles, tendons, and bones that support the lower extremity can usually adapt to such an increased work load if training progresses appropriately. However, the following risk factors may predispose to the development of shin splints by leading to increased ground reactive-forces acting on the lower extremity and/or a compromised musculoskeletal support structure: training errors, foot shape/biomechanics, poor conditioning, high body mass index, poor nutrition, and degenerative changes.1,13-16
Symptoms associated with shin splints may include pain over the anterolateral, or the distal two thirds of the posteromedial aspect of the shin.2-6 Usually, these symptoms are present with activity and alleviated with rest.7 However, if the athlete trains throughout pain and a proper treatment program is not initiated, the symptoms and severity of shin splints may progress.
In the 1900s shin splints was initially defined as any type of pain from the hip to the ankle.14 This broad definition seemed appropriate because treatments for lower extremity injuries were rudimentary and relatively ineffective. Throughout the last four decades medical research has led to advancements in understanding the causes, treatment, and prevention of sports injuries. The exact pathophysiology of shin splints remains unknown; however several possible etiologies have been studied.1,17,18
An understanding of the kinesiology, physiology, and anatomy of the lower leg, risk factors associated with shin splints, and a detailed history and physical examination may aid the practitioner in developing a proper treatment and prevention protocol.3,19,20 Most cases can be effectively treated with conservative care.1,21
Anatomy of the Lower Leg
 Long bones, such as the tibia, consist of an outer rigid layer. This external surface consists of several concentric rings of cortical bone that are surrounded by periosteum, a thin layer of dense fibrous connective tissue that is richly supplied by nerves and blood. The periosteum is anchored to the cortical bone by bundles of connective tissue “Sharpey fibers” (figure 1). The periosteum has several functions: it protects the underlying bone, participates in the repair and remodeling process of bone, and is the site of attachment for adjacent muscles.
Long bones, such as the tibia, consist of an outer rigid layer. This external surface consists of several concentric rings of cortical bone that are surrounded by periosteum, a thin layer of dense fibrous connective tissue that is richly supplied by nerves and blood. The periosteum is anchored to the cortical bone by bundles of connective tissue “Sharpey fibers” (figure 1). The periosteum has several functions: it protects the underlying bone, participates in the repair and remodeling process of bone, and is the site of attachment for adjacent muscles.  Muscles consist of bundles of individual fibers (fasciculi) that are surrounded by endomysium, a thin delicate layer of connective tissue. The fibrocartilage strands of the periosteum intertwine with the endomysium of abutting musculature, creating an extensive origin of attachment. At these origins of attachment the underlying cortical bone is rough or thickened due to bone remodeling in response to traction exerted by muscles.22,23
Muscles consist of bundles of individual fibers (fasciculi) that are surrounded by endomysium, a thin delicate layer of connective tissue. The fibrocartilage strands of the periosteum intertwine with the endomysium of abutting musculature, creating an extensive origin of attachment. At these origins of attachment the underlying cortical bone is rough or thickened due to bone remodeling in response to traction exerted by muscles.22,23
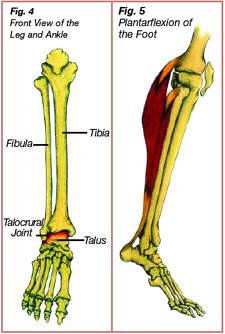
 The tibia has three potential sites for attachments of muscles: a posterior surface, and anterolateral and medial surfaces that are separated by the anterior tibial crest. The soleus, flexor digitorum longus, and tibialis posterior musculature attach to the posterior surface of the tibia (figures 2A). The tibialis anterior musculature attaches to the anterolateral surface of the tibia (figure 2B). These muscles are contained within the superficial posterior, the deep posterior, or the anterior compartment of the leg (figure 3).3,6,24,25 The muscles surrounding the shin aid in coordinating movements of the foot and ankle and in reducing ground reactive forces.
The tibia has three potential sites for attachments of muscles: a posterior surface, and anterolateral and medial surfaces that are separated by the anterior tibial crest. The soleus, flexor digitorum longus, and tibialis posterior musculature attach to the posterior surface of the tibia (figures 2A). The tibialis anterior musculature attaches to the anterolateral surface of the tibia (figure 2B). These muscles are contained within the superficial posterior, the deep posterior, or the anterior compartment of the leg (figure 3).3,6,24,25 The muscles surrounding the shin aid in coordinating movements of the foot and ankle and in reducing ground reactive forces.
Biomechanics of the Lower Leg during Ambulation
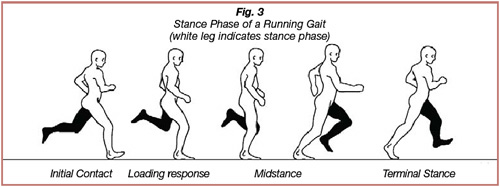
 There are two main phases to a running gait, a stance phaseand a swing phase. During the stance phase the foot contacts and adapts to the ground. The swing phase begins when the stance leg lifts off the ground. Most sport-related injuries can be attributed to repetitive ground reactive forces during the stance phase of gait.26 The stance phase of gait consists of the following sub-phases:
There are two main phases to a running gait, a stance phaseand a swing phase. During the stance phase the foot contacts and adapts to the ground. The swing phase begins when the stance leg lifts off the ground. Most sport-related injuries can be attributed to repetitive ground reactive forces during the stance phase of gait.26 The stance phase of gait consists of the following sub-phases:
- initial contact, when the foot of the swing leg initially contacts the ground.
- loading response, beginning shortly after initial contact as the foot begins to adapt to the ground.
- early midstance, when the contralateral swing leg is midline with the body and distributes the body weight over the stance leg.
- late midstance, starting when the foot of the stance leg changes from a mobile adaptor that absorbs ground reactive forces to a more rigid lever that prepares the foot for toe-off.
- terminal stance, beginning shortly after heel-lift and ending with toe-off (figure 4).27,28,29
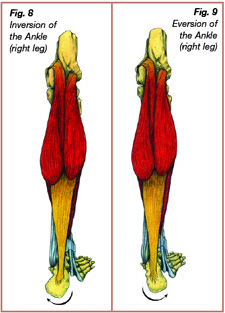
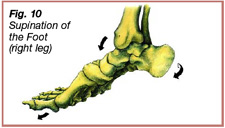
 Throughout loading response and into early midstance, the foot goes through a series of transformations coined “pronation,” allowing the lower extremity to be more efficient in absorbing ground-reactive forces. Pronation of the foot and ankle consists of the following movements:
Throughout loading response and into early midstance, the foot goes through a series of transformations coined “pronation,” allowing the lower extremity to be more efficient in absorbing ground-reactive forces. Pronation of the foot and ankle consists of the following movements:
- 1. The heel bone turns outward (everts), and the medial longitudinal arch (instep arch) lowers toward the ground.
- 2. The tibia approximates to the toes (ground reactive dorsiflexion).
- 3. The forefoot turns outward (abducts) (figure 5).
Normal range of pronation is four degrees of heel eversion and twenty degrees of ground reactive dorsiflexion. Pronation of the foot and ankle should end before late midstance as the foot prepares for toe-off.27,28,30
 Shortly after the foot strikes the ground the muscles attaching to the anterior and posterior aspect of the tibia contract eccentrically; the muscle fibers elongate as tension is produced in an attempt to decelerate a particular motion. The soleus, tibialis posterior, and the flexor digitorum musculature have points of origin on the posterior aspect of the tibia. They contract eccentrically during loading response and into midstance to decelerate pronation. Shortly after initial ground contact, the tibialis anterior muscle contracts eccentrically to decelerate foot slap as the forefoot descends towards the ground (figure 6).24,32
Shortly after the foot strikes the ground the muscles attaching to the anterior and posterior aspect of the tibia contract eccentrically; the muscle fibers elongate as tension is produced in an attempt to decelerate a particular motion. The soleus, tibialis posterior, and the flexor digitorum musculature have points of origin on the posterior aspect of the tibia. They contract eccentrically during loading response and into midstance to decelerate pronation. Shortly after initial ground contact, the tibialis anterior muscle contracts eccentrically to decelerate foot slap as the forefoot descends towards the ground (figure 6).24,32
Under normal circumstances, the musculoskeletal support structures of the lower extremity can adapt to these repetitive eccentric loads. However, training errors, structural abnormalities, and other factors may predispose to excessive eccentric loads placed on the lower leg musculature, resulting in anterolateral or posteromedial shin splints. The exact pathophysiology of shin splints is unknown; however, research has come up with several hypothetical causes.
Possible Etiologies of Shin Splints
Traction Periostitis/Periostalgia
Current research supports the hypothesis that posteromedial shin pain in runners may be caused by excessive eccentric contractions of the superficial and deep posterior compartment muscles that originate on the tibia. Training that does not allow for proper adaptation of the musculoskeletal support structures of the lower leg, due to increased workloads, may lead to inflammation or degenerative changes to the surrounding fascia (fasciitis) or to the periosteum (periostitis/ periostalgia).2,6,26 Currently, medial tibial stress syndrome (MTSS) is the most common term to describe posteromedial shin pain thought to be caused by periostitis or periostalgia.1,19
Anterolateral shin pain has been linked to repetitive eccentric contractions of the tibialis anterior musculature. Downhill running accentuates a more pronounced foot slap, predisposing to fatigue of the tibialis anterior musculature, which may result in anterolateral shin pain due to a similar mechanism of injury as MTSS.14 This paper will define this condition as “anterior tibial stress syndrome” (ATSS).
Bone Stress Reaction
Bone remodeling of the tibia in response to increased work loads commences approximately five days after stimulation.2 Two types of cells are active in bone remodeling: osteoblast cells and osteoclast cells. Osteoblast cells produce new bone, while osteoclast cells react to increased stress by reabsorbing bone. Following bone reabsorption, osteoclast cells secrete osteoid, which is uncalcified bone. Osteoid calcifies into new bone after interacting with calcium and phosphate ions. These adaptations should result in a stronger more rigid skeletal support structure. However, it may take ninety days for the reabsorbed bone to be replaced by mature strong bone.14 Overtraining may lead to a higher ratio of bone reabsorption by osteoclast cells as compared to the production of new bone by osteoblast cells. This may result in a compromised porous skeletal support structure, which is susceptible to a bone stress reaction.1,10,11 Bone stress reactions may include microfractures, or in the more advanced stages a stress fracture. The tibia is the most common location of stress fractures in athletes,19,33,34 and most stress fractures occur four to five weeks after the onset of new exercise.12
The treatment of posteromedial or anterolateral shin splints in minor injuries is similar whether the etiology is traction periostitis/periostalgia or bone stress reaction.1,19 The initial history and physical examination should focus on discovering possible risk factors. Treatment and prevention of shin splints should include steps to eliminate or minimize these risk factors.
Risk Factors Associated with Shin Splints
Risk factors for shin splints are intrinsic (within self) and extrinsic (external to self). 6, 36
Table 1
| Intrinsic Risk Factors | Extrinsic Risk Factors |
| Lower limb structural abnormalities • pes planus (flat foot, which may lead to excessive pronation) • pes cavus (high arch, which may limit pronation and ability to absorb shock) |
Training progression • inappropriate intensity, frequency, or duration of training • hill training that does not progress gradually |
| Poor Conditioning • overweight (body mass index > 30 kg/m2) • insufficient muscle endurance • insufficient muscle strength • limited flexibility |
Gear • unsuitable footwear |
| Female Triad • osteoporosis • amenorrhea • eating disorder |
Training surface • hard uneven ground |
| Age related changes • especially noticeable after 4th decade of life |
Type of sport • activities that involve repetitive running and/or jumping |
| History • previous stress fractures |
1,2,4,10,11,14-16,19,22,33-36,38
A detailed history and physical examination can aid in discovering risk factors that may have contributed to the development of shin splints. Most risk factors are correctable or can be minimized, aiding in the treatment and prevention of future episodes.
Training Guidelines
Recommendations for frequency, duration and intensity of training runs:1,29,39,40
Aerobic Conditioning, 70-80% maximum heart rate (Max HR=220-age):
This level of training is recommended for gradual adaptation to work loads with both cardiovascular conditioning and connective tissue adaptation. Initially, long-distance runners should establish a training base of 4 miles per run at this low intensity level. A progressive training schedule may include a frequency of 4 runs in a 7-day period, generally consisting of 3 shorter runs (each approximately 4-6 miles) during the week, and 1 longer run during the weekend.41 It is recommended that the weekly training mileage should not be increased by more than 10% per week. Based on marathon training logs and personal experience, the duration of the long run is usually increased by an increment of 2 miles per week or every other week, and he intensity should continue at the aerobic conditioning pace. After a proper training base is established, the short duration training runs can be conducted at an increased intensity level.
Anaerobic Conditioning, 80-90% maximum heart rate:
This training is below lactate threshold, the point after which blood lactate rises rapidly, leading to increased ventilation (speaking to a training partner becomes difficult) and eventual muscle fatigue. Anaerobic conditioning training should include a 5 minute warm up, followed by a 15-20 minute duration at the anaerobic conditioning level, then a 1 mile recovery run at the aerobic conditioning pace, followed by another 15-20 minute run at the 80-90% level. Anaerobic training makes running at a submaximal lactate pace easier over a prolonged duration. Ideally, the marathon pace should be conducted slightly below the lactate threshold. Towards the end of the race, “the last kick,” the pace can be increased.
Aerobic Capacity Training (intervals), 90-95% maximum heart rate:
This training is a vigorous challenge to the athlete’s aerobic and anaerobic capabilities, and stimulates slow twitch and fast twitch muscle fibers. This pace should only be maintained for 6-9 minutes, followed by a 4-5 minute recovery run at a slow pace. Aerobic capacity training runs elevate the lactate threshold and condition the body to deal more efficiently with oxygen debt and muscle fatigue.
Other Training Tips:
Add uphill training gradually. Running uphill should be conducted at a slower pace because of increased energy expenditure due to increased arm and shoulder action, and hipflexor and knee lift. Uphill running also predisposes to an increased eccentric strain on the posterior calf musculature. Downhill running should be limited because of increased risk and limited benefits.40,42
Change running shoes every 300-500 miles (approximately every 3-4 months). A sneaker loses approximately 50% of its ability to absorb ground reactive forces after 300-500 miles.1,19,37,43,44
Modify training. Add exercises such as swimming, bicycling, and using an elliptical machine on non-running days, or while recovering from an injury. For prevention of injury, the older athlete (after 4th decade of life) may limit running on pavement.1,4,11,30,45
Implement an eccentric strength training program for the lower leg musculature. This program can aid in the treatment and prevention of injury.76 Standing and seated calf raises strengthen the gastrocnemius, soleus, and the intrinsic musculature of the foot. A dorsiflexionassisted resistive device, resistive tubing, or a cable machine strengthens the tibialis anterior and extensor musculature of the leg.1,4,30,35,43,46,47 The strength training program should address the whole lower kinetic chain.4 Squats eccentrically strengthen the quadriceps, hamstrings, and gluteal musculature; romanian deadlifts eccentrically strengthen the latter two muscles. Abduction, adduction, and hip extension exercises can be conducted with a cable machine or tubing.48 Based on my training experience, this lower extremity routine should be conducted at a frequency of one time per week, usually on a Tuesday, Wednesday, or Thursday, if the long run is conducted on a Saturday or Sunday.
Stretch. Static stretching and ballistic stretching have both been shown to increase flexibility of the lower extremity.49,50 I have found a post-workout stretching routine to be helpful in decreasing cramping and muscle soreness, especially after a long duration training run or bike ride.
Introduce pre-season conditioning. Pre-season conditioning that includes a plyometric program can jump-start the process of bone remodeling and prepare the lower extremity support structures for elevated eccentric work loads.2,6,14,15,26,51,76
It should be emphasized that every athlete needs to be addressed individually. Generic marathon training schedules are helpful, however they may need to be modified for each individual to maximize gains and minimize injury. An experienced trainer may aid the athlete in achieving goals by tailoring a training program and re-assessing progress based on training logs and exertion levels.
Following the above training advice may prevent injury. However, additional treatment and training modification may be necessary for the athlete who experiences shin pain. The discouraged athlete will usually seek care when an injury makes training impossible.
Diagnosing Shin Splints
To properly diagnose the athlete’s condition, the treating physician will take a detailed history and examination to discover the onset and location of pain and attributed risk factors. Palpation may reveal diffuse tenderness over the distal two thirds of the posteromedial aspect of the shin (MTSS) or the anterolateral aspect of the shin (ATSS).16,19,37 However, palpation that reveals the following may be a red flag for bone-stress reaction:
- focal tenderness localized to bone
- swelling
- warmth / redness
- inability to train due to severe pain at the localized sight.14,17,19
Plain film radiographs (x-rays) are routinely taken of the leg in patients with shin pain. This baseline study may reveal a periosteal reaction, callus formation, or a radiolucent line that are common findings of a bone stress reaction or frank stress fracture. Radiographs may also rule out other pathological conditions such as an osteoid osteoma, osteosarcoma, or Ewing’s sarcoma. However, bone stress reactions are usually not visualized on radiographs until the 2nd to 6th week post injury/initial complaints of symptoms.1,21,35,52 “The sensitivity of early fracture detection by radiography can be as low as 15%, and follow up radiographs may demonstrate diagnostic findings in only 50% cases.”16 More advanced studies may be needed for further evaluation, such as an MRI (magnetic resonance imaging test) or a BS (bone scan). These studies are more sensitive in detecting bone pathology earlier in the stage of injury, and they aid clinical judgment in regards to a gradual return to sport specific training. Such gradual returns may require a longer period of modified rest, immobilization, or corrective surgery for more advanced cases of bone stress reactions.1,10,53
Treatment of shin splints
Goals of therapy include the following:
- reduce pain and promote healing.
- incorporate pain-free modified training to maintain fitness.
- correct or minimize risk factors.
- gradually re-introduce pain-free activity.
- develop realistic additional training goals.
Severity of symptoms and level of injury are generally scored on a four-grade system:
Grade 1: Pain is present at the end of the workout but is minimal.
Grade 2: Pain is present during the workout but does not affect performance.
Grade 3: Pain during the workout affects performance but dissipates when the workout ends.
Grade 4: Pain does not allow participation in sport and is present during activities of daily living.1
Usually, the athlete will seek treatment when pain hinders performance. The initial goals of therapy are to promote healing and reduce pain and inflammation. The following initial treatments may be useful:
Inflammation reduction
Use of nonsteroidal anti-inflammatory medications per prescription, and application of a cold pack to the shin for twenty minutes on, one hour off, repeated throughout the day can reduce inflammation. Use of iontophoresis with dexamethasone may also decrease inflammation.1,19,56
Ultrasound and electric muscle stimulation combination therapy
The therapy can restore normal muscle tone, aid in the healing process, and reduce pain.1,10,19,32,57,58
Manual adjustments to the ankle and foot
Adjustments free-up joint motion of the talocrural, subtalar, and midtarsal joint articulations.57,59
Deep tissue procedures, such as the Graston Technique (manual therapy that utilizes specially designed devices) and Active Release Technique (a patented manual therapy technique)
 Procedures break up scar tissue and restore soft tissue motion (figures 7A,7B). There is considerable clinical procedures in treatment of strain/sprain injuries.60-63 Myofascial techniques have been shown to stimulate fibroblast proliferation, leading to collagen synthesis that may promote healing by replacing degenerative tissue with a stronger and more functional tissue.45,65
Procedures break up scar tissue and restore soft tissue motion (figures 7A,7B). There is considerable clinical procedures in treatment of strain/sprain injuries.60-63 Myofascial techniques have been shown to stimulate fibroblast proliferation, leading to collagen synthesis that may promote healing by replacing degenerative tissue with a stronger and more functional tissue.45,65
Phototherapy, such as low-level laser therapy or infrared light
Phototherapy decreases inflammation, increases the speed of tissue healing, and decreases pain.58,64
The above treatments may reduce pain and inflammation, and may speed the body’s normal healing response. However, time is a primary factor in recovery: Approximate return to pre-injury strength for bones, ligaments, muscles, and tendons can range from 12 weeks, 40-50 weeks, 6 weeks-6 months, and 40-50 weeks respectively.1,19
During the initial treatment phase – for more severe Grade 2, Grade 3, and Grade 4 injuries – athletes can maintain cardiovascular fitness with modified training. For example, a runner should cycle or swim at a pain-free level.1,12,19
There are no exact studies indicating when to re-introduce sport-specific training; however, the following may be a useful guideline: If there are no time-specific training goals, cease sport specific activity for 2 weeks, and maintain cardiovascular fitness with modified training. After 2 weeks of modified training and conservative therapy, re-introduce pain-free running on a soft track or treadmill, at approximately 50% of the pre-injury intensity and duration. Then, increase the duration of the training runs by 10% each week. It is hopeful that the pre-injury duration can be reached in 5-6 weeks. Athletes should cease running if they experience pain. A brief period of modified training and resumption of pain-free running at a lower intensity and shorter duration may be necessary. The intensity of the training should progress appropriately only after the pre-injury duration is obtained.37,19
Depending on the duration of the athlete’s most recent pre-injury training run, my recommendations for return to activity may vary with the above guidelines. Usually the duration of the initial training run would be 2-4 miles, conducted on a treadmill, at a speed of 10 minute/mile (very slow for most athletes). If the athlete can conduct 2-3 of these traning runs without pain, we would create a program, based on the above guidelines, for achieving time-specific goals.
Before re-introducing sport-specific training, the following methods may reduce the workload placed on the musculoskeletal support structure of the lower leg that are present due to intrinsic risk factors:
- Buy proper running shoes. A pes cavus foot structure may benefit from a cushioned sneaker. The sneaker liner can be removed and replaced with a cushioned insole. The rearfoot varus, pes planus valgus, and forefoot varus foot structure may benefit from a motion-control sneaker.66
- Use appropriate arch supports as necessary. A semirigid orthosis with a medial arch support, no higher than five-eighths of an inch, can limit excess or prolonged pronation.1,2,27,28,35,67-70
- Tape the foot. Taping can limit pronation.57,71,72
- Temporarily use a quarter-inch or three-quarter inch heel lift.
Temporary use can limit compensatory pronation caused by ankle equinous. As range of motion of the talocrural joint in dorsiflexion improves with therapy, the heel lifts can be removed.1,28,68
- Apply a shin sleeve or strapping. Sleeves and strappings can add support for leg muscles.
- Obtain nutritional advice. A dietitian can calculate caloric burn rate and develop a meal plan for healthy weight loss, maintenance, and proper nutrition.19
- Obtain medical examinations Primary physicians or gynecologists can rule out deficiencies common in athletes, such as low estrogen, ammenorhea, or low bone density.
- Train for flexibility Increasing flexibility can reduce compensatory pronation due to ankle equinous, and the posterior calf musculature can be stretched.1,35,43,73,74
The treating physician needs to continually re-evaluate the athlete during the course of therapy. If the athlete has time-specific goals, is not responding to conservative care, or symptoms re-appear when sport-specific training is re-initiated, a BS or MRI may be needed. In addition, treatment of slow healing stress fractures may require immobilization with casting or a walking boot for approximately 3-8 weeks.4,10 Pain-free modified training can maintain the athlete’s cardiovascular fitness, and sanity, during this period. Once union of the stress fracture is evident on repeat imaging studies, and pain is not present with ambulation, sport-specific training can be gradually re-introduced.
If non-union of the stress fracture is present on repeat imaging studies after 4-6 months of immobilization and rest, surgery may be necessary. Surgery may include intramedullary nailing, cortical drilling, or excision and bone grafting.1,4,33,75 In recalcitrant cases of MTSS, surgery may include fasciotomy of the posteromedial superficial and the deep fascia of the tibia.1 Posteromedial fasciotomy may aid in alleviating the pull of the soleus and deep posterior calf musculature of the leg on their insertions on the tibia, as well as decreasing pain due to denervation of the periosteum.37,19 Post-fasciotomy studies have indicated good results in regards to reduced shin pain, however many athletes are not able to return to full sport specific training levels.35,75
Conclusion:
Shin splints is one of the most common lower leg sport-related injuries. Risk factors include training errors, foot structure abnormalities, high body-mass index, age-related degenerative changes, poor conditioning, and inadequate calcium intake or estrogen levels. Most cases of shin splints can be treated successfully with conservative care. Conservative treatment includes the following:
- reduction of pain and inflammation
- modified training to maintain cardiovascular fitness
- modifications to gear, such as obtaining new running shoes
- implementation of a strength and flexibility program
- correction of training errors
- a pain-free gradual return to sport-specific activity
- nutritional counseling or hormonal therapy
If the injury does not respond to conservative care, or there is a time-specific training goal, a BS or MRI may be beneficial in the early detection of stress fractures or other pathologies. Other treatment options for recalcitrant shin splints may include prolonged immobilization with pain-free modified training, surgery to promote bone-union, or a fasciotomy.
REFERENCES
1. Reid DC. Sports Injury Assessment and Rehabilitation. New York: Churchill Livingston Inc., 1992.
2. Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. The American Journal of Sports Medicine 2004; 32(3):772-780.
3. Hislop M, Tierney P. Anatomical variations within the deep posterior compartment of the leg and important clinical consequences. Journal of Science and Medicine in Sport 2004; 7(3):392-9.
4. Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med 2004; 23:55-81.
5. Magnusson HI, Westlin NE, Nyquist F, Gardsell P, Seeman E, Karlsson MK. Abnormally decreased regional bone density in athletes with medial tibial stress syndrome. American Journal of Sports Medicine 2001; 29(6):712.
6. Herring K. A plyometic training model used to augment rehabilitation from tibial Fasciitis. Current Sports Medicine Reports 2006; 5(3):147-54.
7. Batt ME, Ugalde V, Anderson MW, Shelton DK. A prospective controlled study of diagnostic imaging for acute shin splints. Medicine & Science in Sports & Exercise 1998; 30(11):1564-1571.
8. Thacker SB, Gilchrist J, Stroup D, Dexter Kimsey C. The prevention of shin splints in sports: a systematic review of literature. Medicine & Science in Sports & Exercise 2002; 34(1):32-40.
9. Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk factors for recurrent stress fractures in athletes. The American Journal of Sports Medicine 2001; 29:304-310.
10. Jensen J. Stress fracture in the world class athlete: a case study. Medicine & Science in Sports & Medicine 1998; 30(6):783-787.
11. Tommasini SM, Nasser P, Schaffler MB, Jepsen KJ. Relationship between bone morphology and bone quality in male tibias: implications for stress fracture risk. Journal of Bone and Mineral Research 2005; 20(8):1372-1380.
12. Wall J, Feller JF. Imaging of Stress Fractures in Runners. Clinics in Sports Medicine 2006; 25:781-802.
13. Sommer HM, Vallentyne SW. Effect of foot posture on the incidence of medial tibial stress syndrome. Medicine & Science in Sports & Exercise 1995; 27(6):800-804.
14. Noakes T. The Lore of Running (4th Edition). Illinois: Human Kinetics, 2003; 803-816.
15. Shaffer RA, Rauh MJ, Brodine SK, Trone DW, Macera CA. Predictors of stress fracture susceptibility in young female recruits. The American Journal of Sports Medicine 2006; 34(1):108.
16. Spitz D, Newberg A. Imaging of stress fractures in the athlete. Radiologic Clinics of North America 2002; 40:313-331.
17. Bhatt R, Lauder I, Finlay DB, Allen MJ, Belton IP. Correlation of bone scintigraphy and histological findings in medial tibial syndrome. British Journal of Sports Medicine 2000; 34:49-53.
18. Magnusson HI, Ahlborg HG, Karlsson C, Nyquist F, Karlsson MK. Low regional tibial bone density in athletes with medial tibial stress syndrome normalizes after recovery from symptoms. American Journal of Sports Medicine 2003; 31(4):596.
19. Edwards PH Jr, Wright ML, Hartman JF. American Journal of Sports Medicine 2005; 33:1241.
20. Bennell K, Crossley K, Jayarajan J, Walton E, Warden S, Kiss SZ, Wrigley T. Ground reaction forces and bone parameters in females with tibial stress fracture. Medicine & Science in Sports & Exercise 2004; 36(3):397-404.
21. Aoki Y, Yasuda K, Tohyama H, Ito H, Minami A. Magnetic resonance imaging in stress fractures and shin splints. Clinical Orthopaedics 2004; 421:26-267.
22. Weineck J. Functional Anatomy in Sports, Second Edition. St. Louis: Mosby-Year Book, 1990.
23. Wheater PR, Burkitt HG, Daniels VG. Functional Histology. New York: Churchill Livingstone, 1987.
24. Banks AS, Downey MS, Martin DE, Miller SJ. Foot and Ankle Surgery. Philadelphia: Lipincott Williams & Wilkins, 2001.
25. Clemente CD. Anatomy: A Regional Atlas of the Human Body (3rd Edition). Baltimore: Urban & Schwarzenberg, 1987.
26. Richie D, DeVries H, Endo C. Shin muscle activity and sports surfaces. Journal of the American Podiatric Association 1993; 83(4):181-190.
27. Michaud TC. Foot orthosis and other forms of conservative foot care. Newton MA: Thomas C Michaud, 1997.
28. Donatelli RA. The biomechanics of the foot and ankle, 2nd Edition. Philadelphia: F.A. Davis, 1996.
29. Norkin CC, Levangie PK. Joint Structure and Function: A Comprehensive Analysis (2nd Edition). F.A. Davis, Philadelphia 1992.
30. Banks AS, Downey MS, Martin DE, Miller SJ. Foot and Ankle Surgery. Philadelphia: Lipincott Williams & Wilkins, 2001.
31. Inman VT. Human Locomotion. Can Med Assoc J. 94:1047, 1996.
32. Chleboun GS, Busic AB, Graham KK, Stuckey HA. Fascicle length change of the human tibialis anterior and vastus lateralis during walking. Journal of Orthopaedic & Sports Physical Therapy 2007; 37(7):372-379.
33. Larson CM, Traina SM, Fischer DA, Arendt EA. Recurrent complete proximal tibial stress fracture in a basketball player. The American Journal of Sports Medicine 2005; 33(12):1914.
34. Pozderac RV. Longitudinal tibial fatigue fracture: an uncommon stress fracture with characteristic features. Clinical Nuclear Medicine 2002; 27(7):475-478.
35. Fredericson M, Wun C. Differential diagnosis of leg pain in the athlete. Journal of the American Podiatric Medical Association 2003; 93(4):321-324.
36. Reinking MF, Austin TM, Hayes AM. Exercise-related leg pain in collegiate cross-country athletes: extrinsic and intrinsic risk factors. Journal of Orthpaedic & Sports Physical Therapy 2007; 37(11):670-678.
37. Kortebein PM, Kaufman KR, Basford JR, Stuart MJ. Medial tibial stress syndrome. Medicine & Science in Sports & Exercise 2000; 32(2):S27-S33.
38. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. British Journal of Sports Medicine 2002; 36:95-101.
39. Smurawa T. Overuse injuries curb triathlon preparation efforts. Biomechanics 2006; 13(5).
40. Martin DE, Coe PN. Better Training for Distance Running (2nd Edition). Champaign, IL: Human Kinetics, 1997.
41. Higdon H. Hal Higdon’s Marathon Training Guide. www.halhigdon.com/marathon/Mar00novice.htm. Accessed March 14, 2008.
42. Armstrong RB, Ogilvie RW, Schwane JA. Eccentric exercise-induced injury to rat skeletal muscle. Journal of Applied Physiology 1983; 54(1):80-93.
43. Roxas M. Plantar fasciitis: diagnosis and therapeutic considerations. Alternative Medicine Review 2005; 10(2):83-93.
44. Messier SP, Edwards DG, Martin DF, et al. Etiology of iliotibial band friction syndrome in distance runners. Medicine & Science in Sports & Exercise 2995; 27(7):951-960.
45. Dyck D, Boyajian-O’Neill L. Plantar Fasciitis. Clinical Journal of Sports Medicine 2004; 14(5):305-309.
46. Friden J, Sfakianos PN, Hargens AR. Muscle soreness and intramuscular fluid pressure: comparison between eccentric and concentric load. Journal of Applied Physiology 1986; 61(6):2175-2179.
47. Allen RH, Gross MT. Toe flexors strength and passive extension range of motion of the first metatarsophalangeal joint in individuals with plantar fasciitis. Journal of Orthopaedic & Sports Physical Therapy 2003; 33(8):468-78.
48. reference for squats-muscle activity
49. Witvrouw E, Mahieu N, Roosen P, McNair P. The role of stretching in tendon injuries. British Journal of Sports Medicine 2007; 41:224-226.
50. Witvrouw E, Mahieu N, Danneels L, McNair P. Stretching and injury prevention. Sports Med 2004; 34(7):443:449.
51. Chmielewski TL, Myer GD, Kauffman D, Tillman SM. Plyometric exercise in the rehabilitation of athletes: physiological responses and clinical application. Journal of Orthopaedic & Sports Physical Therapy 2006; 36(5): 308-319.
52. Ruohola JPS, Kiuru MJ, Pihlajamaki HK. Fatigue bone injuries causing anterior lower leg pain. Clinical Orthpaedics and Related Research 2006; 444:216-223.
53. Gaeta M, Minutoli F, Vinci S, Salamone I, D’Andrea Letterio, Bitto L, Magaudda L, Blandino A. High-resolution CT grading of tibial stress reactions in distance runners. American Journal of Radiology 2006; 187:789-793.
54. Hod N, Ashkenazi I, Levi Y, Fire G, Drori M, Cohen I, Bernstine H, Horne T. Characteristics of skeletal stress fractures in female military recruits of the Israeli Defense Forces on bone scintigraphy. Clinial Nuclear Medicine 2006; 31(12):742-749.
55. Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics 2003; 23:341-358.
56. Pellecchia GL, Hamel H, Behnke P. Treatment of infrapatellar tendonitis: a combination of modalities and transverse friction massage versus iontophoresis. J Sports Rehabil 1994; 3(2):35-145.
57. Hyde T. Conservative management of sports injury. Baltimore: Williams & Wilkins, 1997; pp477-82.
58. Gum SL, Reddy GK, Stehno-Bittel L, Enwemeka CS. Combined ultrasound, electrical muscle stimuation, and laser promote collagen synthesis with moderate changes in tendon biomechanics. Am J Phys Med Rehabil 1997; 76(4):288-96.
59. Young B, Walker M, Strunce J, Boyles R. A combined treatment approach emphasizing impairment-based manual physical therapy for plantar heel pain: a case series. The Journal of Orthopaedic & Sports Physical Therapy 2004; 34(11):725-33.
60. Walker JM. Deep transverse frictions in ligament healing. Journal of Orthopaedic & Sports Physical Therapy 1984; 6(2):89-94.
61. Brosseau L, Casimiro, Milne S, et al. Deep transverse friction massage for healing tendonitis. Cochrane Database Syst Rev 2002; (4):CD003528.
62. Kvist M, Jarvinen M. Clinical histochemical and biomechanical features in repair of muscle and tendon injuries. Int J Sports Med 1982; 3 Suppl 1:12-14.
63. Roniger LR. Massage, strengthening reduce knee OA pain disability. Biomechanics 2007; XIV(2): 17-18.
64. Roniger LR. Research focus on lower limb pain brings relief. Biomechanics 2008; XV(1):21.
65. Leadhetter W. Cell matrix response in tendon injury. Clinics in Sports Medicine 1997; 11(3): 533-79.
66. Butler R, Davis I, Hamill J. Interaction of joint type and footwear on running mechanics. The American Journal of Sports Medicine 2006; 34(12):1998-2005.
67. Fillipou D, Kalliakmanis A, Triga A, Rizos A, Grigoriadis E. Sports related plantar fasciitis. Current Diagnostic and Therapeutic Advances. Folia Medica 2004; 46(3):56-60.
68. Sobel E, Levitz S, Caselli M. Orthoses in the treatment of rearfoot problems. Journal of the American Podiatric Association 1999; 89(5):220-33.
69. Landorf K, Keenan A, Herbert R. Effectiveness of different types of foot orthoses for the treatment of plantar fasciitis. Journal of the American Podiatric Association 2004; 94(6):542-49.
70. Kogler G, Veer F, Solomonidis S, Paul J. The influence of medial and lateral placement of orthotic wedges on loading of the plantar aponeurosis: an in vitro study. Journal of Bone & Joint surgery 1999; 81-A(1):1403-1413.
71. Landorf K, Radford J, Keenan A, Redmond A. Effectiveness of low-dye taping for the short term management of plantar fasciitis. Journal of the American Podiatric Association 2005; 95(6):525-30.
72. Radford J, Burns J, Buchbinder R, Landorf K, Cook C. The effect of low-dye taping on the kinematic, kinetic, and electromyographic variables. Journal of Orthopaedic & Sports Physical Therapy 2006; 36(4):232-41.
73. Didiovanni B, Nawoczenski D, Lintal M, Moore E, Murray J, Wilding G, Baumhauer J. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective randomized study. The Journal of Bone & Joint Surgery 2003; 85-A(7):1270-77.
74. Mahieu N, McNair P, DeMuynck M, Stevens V, Blanckaert I, Smits N, Witrouw E. Effect of static and ballistic stretching on the muscle-tendon tissue properties. Medicine & Science in Sports & Exercise 2007; 39(3):494-501.
75. Yates B, Allen MJ, Barnes MR. Outcome of surgical treatment of medial tibial stress syndrome. The Journal of Bone & Joint Surgery 2003; 85- A(10):1974-1980.
76. Woodley BL, Newsham-West RJ, Baxter GD. Chronic tendinopathy: effectiveness of eccentric exercise. British Journal of Sports Medicine 2007; 41:188-199.
77. Andrew JR, Harrelson GL, Wilk KE. Physical rehabilitation of the injured athlete (3rd Edition). Philadelphia, PA:Saunders, 2004.
78. Comfort P. Kasim P. Optimizing squat technique. Strength and Conditioning Journal 2007; 29(6):10-13.
Special thanks to Audrey Mahoney for creating the illustrations.
*To be published in BioMechanics, May/June 2008. ©2008 Dubin Chiropractic
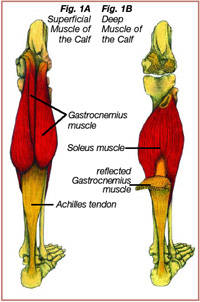 The Achilles tendon, which runs from the top of the heel to the back of the calf, is a strong, non-elastic, fibrous tissue that attaches the gastrocnemius muscle (Figure 1A) and the soleus muscle (Figure 1B) to the calcaneus (heel bone) (1). Another name for the muscle group sharing the Achilles tendon is the “triceps surae.” The Achilles tendon can effectively absorb ground reactive forces associated with running that can approach 6-8 times body weight with an average of 800 foot strikes per mile (2, 23). Injury to the Achilles tendon or its surrounding sheath, the paratendon, can be the result of overuse, improper training, gait abnormalities, age related degenerative changes, or improper footwear (1-7). Recreational runners who prematurely increase the intensity, duration, and/or frequency of their training sessions are prone to developing Achilles tendon injuries because the Achilles tendon does not have the time to adapt to the increased demand. Improper training may lead to microtears and degenerative changes to the Achilles tendon or the surrounding paratendon, weakening the tendon and predisposing it to further injury. Achilles tendon injuries usually occur gradually, increasing in severity without proper treatment and rehabilitation. Symptoms of Achilles tendon injuries can include one or more of the following:
The Achilles tendon, which runs from the top of the heel to the back of the calf, is a strong, non-elastic, fibrous tissue that attaches the gastrocnemius muscle (Figure 1A) and the soleus muscle (Figure 1B) to the calcaneus (heel bone) (1). Another name for the muscle group sharing the Achilles tendon is the “triceps surae.” The Achilles tendon can effectively absorb ground reactive forces associated with running that can approach 6-8 times body weight with an average of 800 foot strikes per mile (2, 23). Injury to the Achilles tendon or its surrounding sheath, the paratendon, can be the result of overuse, improper training, gait abnormalities, age related degenerative changes, or improper footwear (1-7). Recreational runners who prematurely increase the intensity, duration, and/or frequency of their training sessions are prone to developing Achilles tendon injuries because the Achilles tendon does not have the time to adapt to the increased demand. Improper training may lead to microtears and degenerative changes to the Achilles tendon or the surrounding paratendon, weakening the tendon and predisposing it to further injury. Achilles tendon injuries usually occur gradually, increasing in severity without proper treatment and rehabilitation. Symptoms of Achilles tendon injuries can include one or more of the following: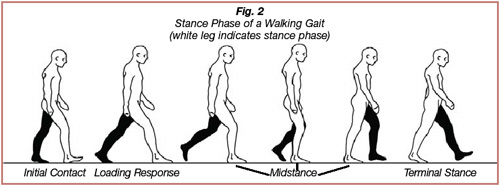
 There are two types of active muscle contractions: eccentric and concentric. An eccentric contraction involves lengthening of a muscle as it attempts to decelerate a particular movement, while a concentric contraction involves shortening of a muscle as it generates force to produce movement across a joint. Most overuse soft tissue injuries are caused by repetitive eccentric forces that exceed the tensile strength of the tissue that is attempting to decelerate a particular movement. The Achilles tendon is the strongest tendon in the body; normally it does not incur injury when absorbing the eccentric forces exerted on it during running or jumping (1). However certain gait abnormalities, tightness of the calf musculature, improper training, and age-related changes can predispose the Achilles tendon to repetitive microtrauma and injury.
There are two types of active muscle contractions: eccentric and concentric. An eccentric contraction involves lengthening of a muscle as it attempts to decelerate a particular movement, while a concentric contraction involves shortening of a muscle as it generates force to produce movement across a joint. Most overuse soft tissue injuries are caused by repetitive eccentric forces that exceed the tensile strength of the tissue that is attempting to decelerate a particular movement. The Achilles tendon is the strongest tendon in the body; normally it does not incur injury when absorbing the eccentric forces exerted on it during running or jumping (1). However certain gait abnormalities, tightness of the calf musculature, improper training, and age-related changes can predispose the Achilles tendon to repetitive microtrauma and injury.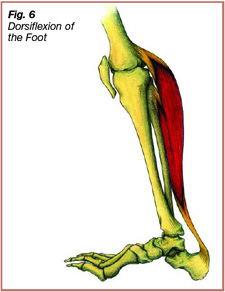 During the midstance phase of gait, the triceps surae contracts eccentrically, exerting force through the Achilles tendon to decelerate forward movement of the stance leg over the foot (2, 4, 14). Dorsiflexion of the ankle joint is dependent on flexibility of the triceps surae. A tight tricep surae limits dorsiflexion of the ankle joint, placing excessive eccentric strain on the Achilles tendon throughout midstance, predisposing it and the surrounding paratendon to injury.
During the midstance phase of gait, the triceps surae contracts eccentrically, exerting force through the Achilles tendon to decelerate forward movement of the stance leg over the foot (2, 4, 14). Dorsiflexion of the ankle joint is dependent on flexibility of the triceps surae. A tight tricep surae limits dorsiflexion of the ankle joint, placing excessive eccentric strain on the Achilles tendon throughout midstance, predisposing it and the surrounding paratendon to injury.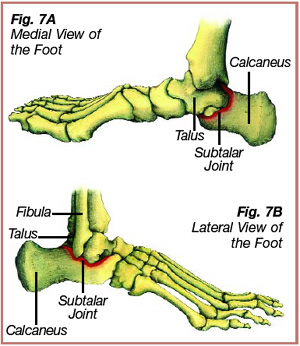
 During initial contact the calcaneus is normally in 2-3 degrees of inversion. However, certain structural abnormalities can change normal inversion. One such structural abnormality, rearfoot varus, involves excessive inversion of the calcaneus during initial surface contact. To compensate for rearfoot varus, the subtalar joint pronates excessively and at a faster speed than normal to allow for the medial aspect of the calcaneus to contact and adapt to the terrain. The excessive pronation of the subtalar joint, which occurs at an increased velocity from initial contact to midstance, places an increased eccentric load on the Achilles tendon, predisposing the tendon to injury.
During initial contact the calcaneus is normally in 2-3 degrees of inversion. However, certain structural abnormalities can change normal inversion. One such structural abnormality, rearfoot varus, involves excessive inversion of the calcaneus during initial surface contact. To compensate for rearfoot varus, the subtalar joint pronates excessively and at a faster speed than normal to allow for the medial aspect of the calcaneus to contact and adapt to the terrain. The excessive pronation of the subtalar joint, which occurs at an increased velocity from initial contact to midstance, places an increased eccentric load on the Achilles tendon, predisposing the tendon to injury.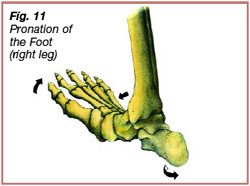 Forefoot varum is another structural abnormality that predisposes the Achilles tendon to injury. In this condition the forefoot has an increased inversion tilt as compared to the rearfoot. Forefoot varum leads to prolonged pronation through midstance and into terminal stance to allow for the inside of the forefoot to contact the ground surface. During the beginning of midstance and into terminal stance of a normal running gait, the subtalar joint re-supinates to change the foot into an effective rigid lever for toe-off. However, a runner’s gait with forefoot varum may exhibit prolonged pronation throughout midstance causing the subtalar joint to rapidly re-supinate and create a rigid lever for toe-off. Prolonged pronation into midstance followed by an attempt of the subtalar joint to re-supinate causes a bowstring effect on the Achilles tendon (Figure 12). The bowstring effect places an increased eccentric load on the medial side of the Achilles tendon, predisposing it to injury (5, 15, 23, 24).
Forefoot varum is another structural abnormality that predisposes the Achilles tendon to injury. In this condition the forefoot has an increased inversion tilt as compared to the rearfoot. Forefoot varum leads to prolonged pronation through midstance and into terminal stance to allow for the inside of the forefoot to contact the ground surface. During the beginning of midstance and into terminal stance of a normal running gait, the subtalar joint re-supinates to change the foot into an effective rigid lever for toe-off. However, a runner’s gait with forefoot varum may exhibit prolonged pronation throughout midstance causing the subtalar joint to rapidly re-supinate and create a rigid lever for toe-off. Prolonged pronation into midstance followed by an attempt of the subtalar joint to re-supinate causes a bowstring effect on the Achilles tendon (Figure 12). The bowstring effect places an increased eccentric load on the medial side of the Achilles tendon, predisposing it to injury (5, 15, 23, 24).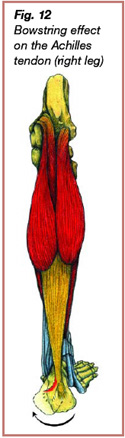 The subtalar joint in a runner with a flat inside arch (pes planus) tends to overpronate, causing an increased eccentric strain on the Achilles tendon. The subtalar joint in a runner with a rigid high inside arch (pes cavus) has limited pronation. Limited pronation decreases the ability of the foot and ankle to absorb ground forces, leading to transmission of excessive forces through the Achilles tendon and other adjacent structures.
The subtalar joint in a runner with a flat inside arch (pes planus) tends to overpronate, causing an increased eccentric strain on the Achilles tendon. The subtalar joint in a runner with a rigid high inside arch (pes cavus) has limited pronation. Limited pronation decreases the ability of the foot and ankle to absorb ground forces, leading to transmission of excessive forces through the Achilles tendon and other adjacent structures.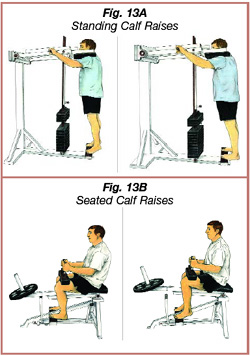 4. Inflammation reduction by icing the Achilles tendon for 20 minutes on, 1 hour off, repeating throughout the day, and use of NSAIDs (non-steroidal anti-inflammatory drugs) per primary doctor recommendation. Iontophoresis with dexamethasone is also a useful modality to decrease inflammation.
4. Inflammation reduction by icing the Achilles tendon for 20 minutes on, 1 hour off, repeating throughout the day, and use of NSAIDs (non-steroidal anti-inflammatory drugs) per primary doctor recommendation. Iontophoresis with dexamethasone is also a useful modality to decrease inflammation.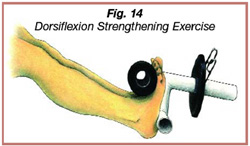 7. A recommendation to replace running sneakers after 250-400 miles of use, at which point the shoe loses 40% of its shock absorption abilities.
7. A recommendation to replace running sneakers after 250-400 miles of use, at which point the shoe loses 40% of its shock absorption abilities.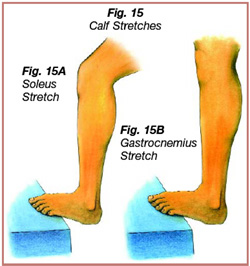 9. A night splint that maintains the ankle and foot in slight dorsiflexion can help to alleviate morning stiffness in the Achilles tendon (23). For more advanced cases of Achilles tendon injury a walking splint can alleviate stress on the slowly healing tendon.
9. A night splint that maintains the ankle and foot in slight dorsiflexion can help to alleviate morning stiffness in the Achilles tendon (23). For more advanced cases of Achilles tendon injury a walking splint can alleviate stress on the slowly healing tendon.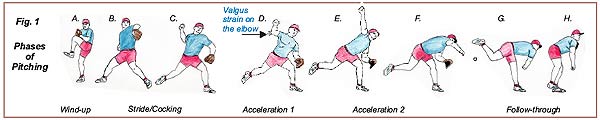
 The power of the pitch is transferred from the torso and lower trunk to the shoulder, arm, and hand during acceleration 2 (Figs. 1E-F). During this phase, the trunk springs from extension (stretching out) to flexion (bending in) and rotates towards home plate over the planted stride leg. At the same time, the shoulder rotates internally and the arm and hand accelerate towards the plate until the baseball is released from the hand.
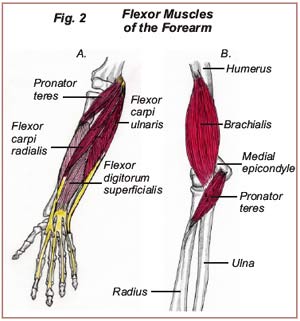
The power of the pitch is transferred from the torso and lower trunk to the shoulder, arm, and hand during acceleration 2 (Figs. 1E-F). During this phase, the trunk springs from extension (stretching out) to flexion (bending in) and rotates towards home plate over the planted stride leg. At the same time, the shoulder rotates internally and the arm and hand accelerate towards the plate until the baseball is released from the hand.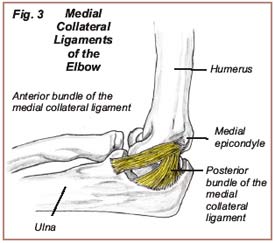 During the cocking and acceleration 1 phases, the wrist is slightly extended, stretching the flexor muscles of the forearm-the flexor digitorum superficialis, flexor carpi radialis, and flexor carpi ulnaris (Fig. 2A)-and an increased “valgus strain” is placed on the medial collateral ligament. From acceleration 1 to acceleration 2, the wrist goes from a slightly extended position to a flexed position, causing a forceful contraction of the forearm flexors. The tendons attached to these forearm flexors have a common insertion point on the medial epicondyle, an outgrowth of bone found on the inside and bottom of the humerus (arm bone). When these muscles are under-prepared and stretched in this way, tension develops in the tendons at the insertion point on the medial epicondyle. Overuse may cause microtears in these structures, causing pain at the medial epicondyle in the elbow.
During the cocking and acceleration 1 phases, the wrist is slightly extended, stretching the flexor muscles of the forearm-the flexor digitorum superficialis, flexor carpi radialis, and flexor carpi ulnaris (Fig. 2A)-and an increased “valgus strain” is placed on the medial collateral ligament. From acceleration 1 to acceleration 2, the wrist goes from a slightly extended position to a flexed position, causing a forceful contraction of the forearm flexors. The tendons attached to these forearm flexors have a common insertion point on the medial epicondyle, an outgrowth of bone found on the inside and bottom of the humerus (arm bone). When these muscles are under-prepared and stretched in this way, tension develops in the tendons at the insertion point on the medial epicondyle. Overuse may cause microtears in these structures, causing pain at the medial epicondyle in the elbow.
 Patellofemoral Syndrome (PFS), pain in the front of the knee, is one of the most common complaints of athletes and active people. PFS is typically caused by a repetitive strain injury or a single traumatic event. Repetitive strain injuries occur when micro-tears in the muscles, tendons and ligaments surrounding the knee joint occur faster then tissue repair, while a single event is often a fall or other athletic impact. PFS is usually characterized by a dull aching pain on the front, bottom, or top of the knee, sometimes accompanied by swelling of the knee joint. Failure to treat this injury appropriately may lead to increased pain symptoms, further damage to the structures stabilizing the knee joint, and eventually an inability of the injured knee to support body weight. This syndrome commonly occurs in athletes or the “weekend warrior” participating in sports such as basketball, football, soccer, triathlons, or track and field events. These sports involve repetitive running, jumping and sometimes kicking, placing a lot of tension on the structures supporting the knee joint.
Patellofemoral Syndrome (PFS), pain in the front of the knee, is one of the most common complaints of athletes and active people. PFS is typically caused by a repetitive strain injury or a single traumatic event. Repetitive strain injuries occur when micro-tears in the muscles, tendons and ligaments surrounding the knee joint occur faster then tissue repair, while a single event is often a fall or other athletic impact. PFS is usually characterized by a dull aching pain on the front, bottom, or top of the knee, sometimes accompanied by swelling of the knee joint. Failure to treat this injury appropriately may lead to increased pain symptoms, further damage to the structures stabilizing the knee joint, and eventually an inability of the injured knee to support body weight. This syndrome commonly occurs in athletes or the “weekend warrior” participating in sports such as basketball, football, soccer, triathlons, or track and field events. These sports involve repetitive running, jumping and sometimes kicking, placing a lot of tension on the structures supporting the knee joint. The patella, or kneecap, is a conical shaped bone lying between the femur (thigh) bone and the tibia (lower leg) bone (Fig.1). The undersurface of the patella glides over the trochlea, a groove located at the bottom and front of the femur bone. The quadricep muscle group, which plays a vital role in the stability of the knee, is located on the front of the thigh and consists of four muscles, the vastus lateralis, vastus intermedius, vastus medialis and the overlying rectus femoris (Fig. 2). The quadricep muscles share a common tendon, the quadricep tendon, which anchors these muscles onto the top of the patella. The patella ligament acts as a downward continuation of the quadricep tendon, originating from the bottom of the patella and inserting onto the tibial tuberosity, an outgrowth of bone on the front of the tibia.
The patella, or kneecap, is a conical shaped bone lying between the femur (thigh) bone and the tibia (lower leg) bone (Fig.1). The undersurface of the patella glides over the trochlea, a groove located at the bottom and front of the femur bone. The quadricep muscle group, which plays a vital role in the stability of the knee, is located on the front of the thigh and consists of four muscles, the vastus lateralis, vastus intermedius, vastus medialis and the overlying rectus femoris (Fig. 2). The quadricep muscles share a common tendon, the quadricep tendon, which anchors these muscles onto the top of the patella. The patella ligament acts as a downward continuation of the quadricep tendon, originating from the bottom of the patella and inserting onto the tibial tuberosity, an outgrowth of bone on the front of the tibia. There are three main types of muscle contractions: concentric, eccentric, and isometric. Each of these contractions may contribute to PFS in different ways. During a concentric contraction, a muscle shortens to perform a particular motion. The patella, quadricep muscle, quadricep tendon, and patella ligament create the “extensor mechanism” of the knee. When the quadricep muscles concentrically contract, they pull on the quadricep tendon, causing tension on the patella and patella ligament, leading to extension of the leg (Figure 4C). An athlete’s ability to kick a soccer ball or football is dependent on the concentric strength of the quadricep muscles and also on the flexibility of the hamstring musculature. The hamstring muscle group acts to decelerate extension of the leg. Inadequate flexibility of the hamstring musculature will place an increased strain on the quadricep muscles during leg extension, predisposing the athlete to the development of PFS.
There are three main types of muscle contractions: concentric, eccentric, and isometric. Each of these contractions may contribute to PFS in different ways. During a concentric contraction, a muscle shortens to perform a particular motion. The patella, quadricep muscle, quadricep tendon, and patella ligament create the “extensor mechanism” of the knee. When the quadricep muscles concentrically contract, they pull on the quadricep tendon, causing tension on the patella and patella ligament, leading to extension of the leg (Figure 4C). An athlete’s ability to kick a soccer ball or football is dependent on the concentric strength of the quadricep muscles and also on the flexibility of the hamstring musculature. The hamstring muscle group acts to decelerate extension of the leg. Inadequate flexibility of the hamstring musculature will place an increased strain on the quadricep muscles during leg extension, predisposing the athlete to the development of PFS.
 Flexibility and strength training of the hamstring musculature and the nearby muscles surrounding the pelvis and thigh will reduce the risk of injury. Strengthening the abdominal and gluteus maximus musculature is important in the prevention of a hamstring strain because these muscles aid the hamstrings in decelerating flexion of the pelvis during heel strike. Flexibility of the hip flexors and low back musculature is also important in the prevention of a hamstring strain injury. Tight hip flexors and low back musculature causes excessive flexion of the pelvis during foot-strike placing an increased strain on the hamstrings. Tightness in these muscles also inhibits strengthening of the gluteus maximus and abdominal musculature.
Flexibility and strength training of the hamstring musculature and the nearby muscles surrounding the pelvis and thigh will reduce the risk of injury. Strengthening the abdominal and gluteus maximus musculature is important in the prevention of a hamstring strain because these muscles aid the hamstrings in decelerating flexion of the pelvis during heel strike. Flexibility of the hip flexors and low back musculature is also important in the prevention of a hamstring strain injury. Tight hip flexors and low back musculature causes excessive flexion of the pelvis during foot-strike placing an increased strain on the hamstrings. Tightness in these muscles also inhibits strengthening of the gluteus maximus and abdominal musculature.
 Most people suffer from low back pain at some time in their lives. Common cases of low back pain include people who work in a prolonged flexed posture while sitting at a computer, or the “weekend warriors” who attempt to participate in activities such as golf, biking, and basketball without a proper training program.
Most people suffer from low back pain at some time in their lives. Common cases of low back pain include people who work in a prolonged flexed posture while sitting at a computer, or the “weekend warriors” who attempt to participate in activities such as golf, biking, and basketball without a proper training program.
 Carpal tunnel syndrome is a common occupational injury resulting from tasks that involve repetitive extension and flexion of the fingers, such as typing on a computer keyboard (Fig. 1).
Carpal tunnel syndrome is a common occupational injury resulting from tasks that involve repetitive extension and flexion of the fingers, such as typing on a computer keyboard (Fig. 1).
 Each step can be broken down into two phases: the stance phase and the swing phase. The stance phase occurs when the foot is making contact with the ground surface. This phase can be divided into three periods: the contact period, mid stance period, and propulsive period (Fig. 1). The second phase is the swing phase, which occurs after toe off and before heel strike, when the leg is not in contact with the ground surface.
Each step can be broken down into two phases: the stance phase and the swing phase. The stance phase occurs when the foot is making contact with the ground surface. This phase can be divided into three periods: the contact period, mid stance period, and propulsive period (Fig. 1). The second phase is the swing phase, which occurs after toe off and before heel strike, when the leg is not in contact with the ground surface.
 Treatment of Walter’s plantar fasciitis consisted of specialized muscle work to free up soft tissue motion of the foot and surrounding musculature. Adjustments were utilized to free up joint motion in the foot and ankle, and ultrasound and electric stimulation were utilized to relax the musculature and restore normal muscle tone. Walter was advised to follow this plan: a stretching and strengthening exercise routine for the lower extremity using the Flex-Band®; rolling a golf ball under the medial arch of his foot (for ischemic compression therapy of the plantar musculature and fascia [Fig. 3]); and application of ice 20 minutes on, 1 hour off, to decrease inflammation. Dr. Dubin also recommended that he invest in a new pair of running sneakers for good shock absorption and comfort, since sneakers lose about 40% of their shock absorption capabilities after approximately 250 miles; they should be replaced every four to six months.
Treatment of Walter’s plantar fasciitis consisted of specialized muscle work to free up soft tissue motion of the foot and surrounding musculature. Adjustments were utilized to free up joint motion in the foot and ankle, and ultrasound and electric stimulation were utilized to relax the musculature and restore normal muscle tone. Walter was advised to follow this plan: a stretching and strengthening exercise routine for the lower extremity using the Flex-Band®; rolling a golf ball under the medial arch of his foot (for ischemic compression therapy of the plantar musculature and fascia [Fig. 3]); and application of ice 20 minutes on, 1 hour off, to decrease inflammation. Dr. Dubin also recommended that he invest in a new pair of running sneakers for good shock absorption and comfort, since sneakers lose about 40% of their shock absorption capabilities after approximately 250 miles; they should be replaced every four to six months. Iliotibial band friction syndrome is a common knee injury afflicting athletes who participate in sports that involve repetitive flexion (knee bends) and extension (knee straightens out), such as cycling and running. The first symptom of iliotibial band friction syndrome is a mild ache on the outside of the knee. Typically this ache does not hinder training, and the discomfort disappears before the next training session. If training continues without proper treatment, the mild ache the outside of the knee may progress to an intense burning or stabbing sensation, which can then radiate to the outside of the thigh and calf. At this later stage of the injury, the speed and distance of the training runs are decreased because of extreme discomfort with flexion of the knee, and the intensity of the pain may eventually force the athlete to stop training.
Iliotibial band friction syndrome is a common knee injury afflicting athletes who participate in sports that involve repetitive flexion (knee bends) and extension (knee straightens out), such as cycling and running. The first symptom of iliotibial band friction syndrome is a mild ache on the outside of the knee. Typically this ache does not hinder training, and the discomfort disappears before the next training session. If training continues without proper treatment, the mild ache the outside of the knee may progress to an intense burning or stabbing sensation, which can then radiate to the outside of the thigh and calf. At this later stage of the injury, the speed and distance of the training runs are decreased because of extreme discomfort with flexion of the knee, and the intensity of the pain may eventually force the athlete to stop training.