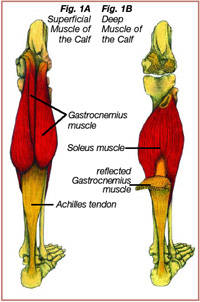
 The Achilles tendon, which runs from the top of the heel to the back of the calf, is a strong, non-elastic, fibrous tissue that attaches the gastrocnemius muscle (Figure 1A) and the soleus muscle (Figure 1B) to the calcaneus (heel bone) (1). Another name for the muscle group sharing the Achilles tendon is the “triceps surae.” The Achilles tendon can effectively absorb ground reactive forces associated with running that can approach 6-8 times body weight with an average of 800 foot strikes per mile (2, 23). Injury to the Achilles tendon or its surrounding sheath, the paratendon, can be the result of overuse, improper training, gait abnormalities, age related degenerative changes, or improper footwear (1-7). Recreational runners who prematurely increase the intensity, duration, and/or frequency of their training sessions are prone to developing Achilles tendon injuries because the Achilles tendon does not have the time to adapt to the increased demand. Improper training may lead to microtears and degenerative changes to the Achilles tendon or the surrounding paratendon, weakening the tendon and predisposing it to further injury. Achilles tendon injuries usually occur gradually, increasing in severity without proper treatment and rehabilitation. Symptoms of Achilles tendon injuries can include one or more of the following:
The Achilles tendon, which runs from the top of the heel to the back of the calf, is a strong, non-elastic, fibrous tissue that attaches the gastrocnemius muscle (Figure 1A) and the soleus muscle (Figure 1B) to the calcaneus (heel bone) (1). Another name for the muscle group sharing the Achilles tendon is the “triceps surae.” The Achilles tendon can effectively absorb ground reactive forces associated with running that can approach 6-8 times body weight with an average of 800 foot strikes per mile (2, 23). Injury to the Achilles tendon or its surrounding sheath, the paratendon, can be the result of overuse, improper training, gait abnormalities, age related degenerative changes, or improper footwear (1-7). Recreational runners who prematurely increase the intensity, duration, and/or frequency of their training sessions are prone to developing Achilles tendon injuries because the Achilles tendon does not have the time to adapt to the increased demand. Improper training may lead to microtears and degenerative changes to the Achilles tendon or the surrounding paratendon, weakening the tendon and predisposing it to further injury. Achilles tendon injuries usually occur gradually, increasing in severity without proper treatment and rehabilitation. Symptoms of Achilles tendon injuries can include one or more of the following:
- diffuse or localized swelling and tenderness around the tendon
- pain with the first few steps after getting out of bed in the morning
- exacerbation of the injury upon walking uphill.
Conservative therapy can aid in the normal reparative processes of Achilles tendon healing, thereby allowing athletes to return to their sport more quickly (4, 8).
There are three classifications of Achilles tendon injuries: tendinosis, tendonitis, and paratenonitis. Achilles tendinosis is a non-inflammatory asymptomatic condition that may lead to abnormal thickening of the tendon or other structural degenerative changes. These degenerative changes compromise the strength and function of the Achilles tendon, predisposing it to further injury. Achilles tendonitis and paratenonitis are painful inflammatory conditions of the Achilles tendon and surrounding paratendon respectively (1, 9, 10, 11).
To develop effective treatments for these injuries, it is necessary to understand the biomechanics of the ankle joint, the function of the triceps surae during a normal running gait, and the conditions that predispose the Achilles tendon to injury.
BIOMECHANICS OF THE ANKLE JOINT AND ACHILLES TENDON WITH RUNNING
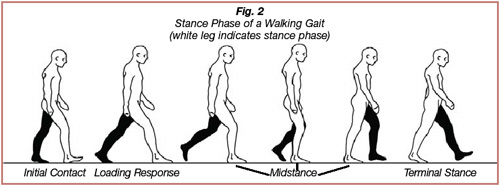
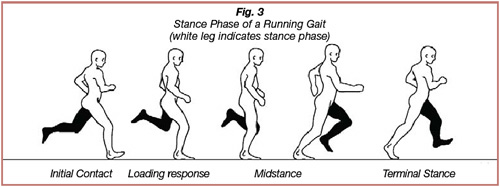
A runner’s gait can be separated into two phases: the stance phase and the swing phase. During the stance phase, the foot contacts and adapts to the ground surface; during the swing phase, the leg accelerates forward and prepares for ground contact. The stance phase with walking consists of the following sub-phases: initial contact, loading response, midstance, and terminal stance (Figures 2). During initial contact, the heel contacts the ground surface. The loading response occurs immediately after initial contact, ending when the contralateral foot lifts off of the ground surface. During the loading response, the foot and ankle adapt to the terrain and absorb ground reactive forces. Double limb support occurs during initial contact and the loading response, when both feet are in contact with the ground surface. The midstance phase starts when the contralateral foot lifts off of the ground surface; the contralateral leg is now the swing leg. The midstance phase ends as the forward momentum of the swing leg and the tension on the triceps surae of the stance leg cause the heel to lift off of the ground surface. The terminal stance phase begins when the heel lifts off of the ground and ends when the swing leg contacts the ground. The running stance phase differs from the walking stance phase in that the stride is elongated, the cadence is increased, and double limb support is eliminated (Figures 3) (6, 12, 13).
 There are two types of active muscle contractions: eccentric and concentric. An eccentric contraction involves lengthening of a muscle as it attempts to decelerate a particular movement, while a concentric contraction involves shortening of a muscle as it generates force to produce movement across a joint. Most overuse soft tissue injuries are caused by repetitive eccentric forces that exceed the tensile strength of the tissue that is attempting to decelerate a particular movement. The Achilles tendon is the strongest tendon in the body; normally it does not incur injury when absorbing the eccentric forces exerted on it during running or jumping (1). However certain gait abnormalities, tightness of the calf musculature, improper training, and age-related changes can predispose the Achilles tendon to repetitive microtrauma and injury.
There are two types of active muscle contractions: eccentric and concentric. An eccentric contraction involves lengthening of a muscle as it attempts to decelerate a particular movement, while a concentric contraction involves shortening of a muscle as it generates force to produce movement across a joint. Most overuse soft tissue injuries are caused by repetitive eccentric forces that exceed the tensile strength of the tissue that is attempting to decelerate a particular movement. The Achilles tendon is the strongest tendon in the body; normally it does not incur injury when absorbing the eccentric forces exerted on it during running or jumping (1). However certain gait abnormalities, tightness of the calf musculature, improper training, and age-related changes can predispose the Achilles tendon to repetitive microtrauma and injury.
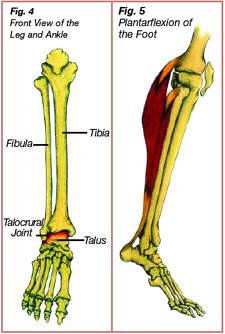
The ankle joint is actually two joints: the talocrural joint and the subtalar joint. The talocrural joint is the articulation between the leg bones (tibia and fibula) and the talus (an ankle bone) (Figure 4). Two types of movements primarily occur at the talocrural joint: plantarflexion and dorsiflexion. Plantarflexion of the talocrural joint involves the toes pointing downwards as the heel lifts off of the ground (Figure 5). Plantarflexion of the ankle joint occurs when conducting a calf raise as the triceps surae contracts concentrically. Dorsiflexion of the ankle joint involves approximation of the leg towards the foot and occurs throughout the midstance phase of gait (Figure 6).
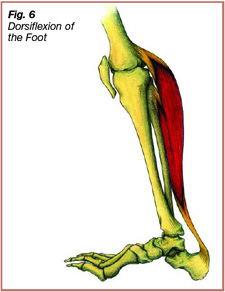 During the midstance phase of gait, the triceps surae contracts eccentrically, exerting force through the Achilles tendon to decelerate forward movement of the stance leg over the foot (2, 4, 14). Dorsiflexion of the ankle joint is dependent on flexibility of the triceps surae. A tight tricep surae limits dorsiflexion of the ankle joint, placing excessive eccentric strain on the Achilles tendon throughout midstance, predisposing it and the surrounding paratendon to injury.
During the midstance phase of gait, the triceps surae contracts eccentrically, exerting force through the Achilles tendon to decelerate forward movement of the stance leg over the foot (2, 4, 14). Dorsiflexion of the ankle joint is dependent on flexibility of the triceps surae. A tight tricep surae limits dorsiflexion of the ankle joint, placing excessive eccentric strain on the Achilles tendon throughout midstance, predisposing it and the surrounding paratendon to injury.
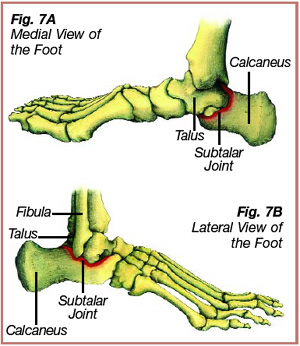
The subtalar joint of the ankle consists of the articulation between the talus and the underlying calcaneus (Figure 7). Two primary movements occur at the subtalar joint: inversion and eversion. Subtalar joint inversion involves the calcaneus turning inward (Figure 8). The ankle joint is stabilized in subtalar inversion as the ligaments and surrounding structures on the outside of the ankle become taut. Inversion of the calcaneus occurs during the initial contact phase to prepare for ground contact, and later in the terminal stance phase to provide a rigid platform for toe-off. Subtalar joint eversion involves the calcaneus turning outward (Figure 9). Eversion of the calcaneus occurs during the loading response and continues into the beginning of midstance. From loading response to midstance the foot and ankle change from a rigid lever into a mobile shock absorber and adapt to the terrain.
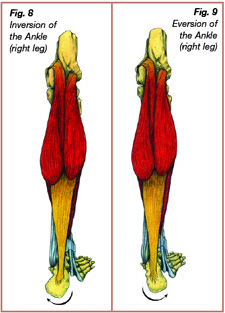
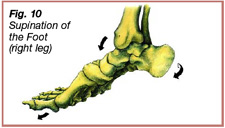
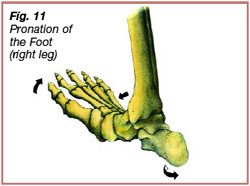
Initially, when the foot strikes the ground, it is in supination; the talocrural joint is neutral and plantarflexing, the subtalar joint is inverted, and the forefoot is adducted – toes are directed towards the midline (Figure 10). The supinated position maintains stability of the ankle joint during initial contact with the ground. After initial contact the ankle pronates, the talocrural joint dorsiflexes, the subtalar joint everts, and the forefoot abducts – toes are pointed away from the midline (Figure 11). The ankle pronates during the loading response and into the beginning of midstance, allowing the ankle and foot to absorb compressive forces and become a mobile adaptor to the ground. During pronation the triceps surae contracts eccentrically to decelerate eversion and dorsiflexion at the ankle joint. The ankle re-supinates during midstance to create a rigid lever for effective toe-off.
 During initial contact the calcaneus is normally in 2-3 degrees of inversion. However, certain structural abnormalities can change normal inversion. One such structural abnormality, rearfoot varus, involves excessive inversion of the calcaneus during initial surface contact. To compensate for rearfoot varus, the subtalar joint pronates excessively and at a faster speed than normal to allow for the medial aspect of the calcaneus to contact and adapt to the terrain. The excessive pronation of the subtalar joint, which occurs at an increased velocity from initial contact to midstance, places an increased eccentric load on the Achilles tendon, predisposing the tendon to injury.
During initial contact the calcaneus is normally in 2-3 degrees of inversion. However, certain structural abnormalities can change normal inversion. One such structural abnormality, rearfoot varus, involves excessive inversion of the calcaneus during initial surface contact. To compensate for rearfoot varus, the subtalar joint pronates excessively and at a faster speed than normal to allow for the medial aspect of the calcaneus to contact and adapt to the terrain. The excessive pronation of the subtalar joint, which occurs at an increased velocity from initial contact to midstance, places an increased eccentric load on the Achilles tendon, predisposing the tendon to injury.
 Forefoot varum is another structural abnormality that predisposes the Achilles tendon to injury. In this condition the forefoot has an increased inversion tilt as compared to the rearfoot. Forefoot varum leads to prolonged pronation through midstance and into terminal stance to allow for the inside of the forefoot to contact the ground surface. During the beginning of midstance and into terminal stance of a normal running gait, the subtalar joint re-supinates to change the foot into an effective rigid lever for toe-off. However, a runner’s gait with forefoot varum may exhibit prolonged pronation throughout midstance causing the subtalar joint to rapidly re-supinate and create a rigid lever for toe-off. Prolonged pronation into midstance followed by an attempt of the subtalar joint to re-supinate causes a bowstring effect on the Achilles tendon (Figure 12). The bowstring effect places an increased eccentric load on the medial side of the Achilles tendon, predisposing it to injury (5, 15, 23, 24).
Forefoot varum is another structural abnormality that predisposes the Achilles tendon to injury. In this condition the forefoot has an increased inversion tilt as compared to the rearfoot. Forefoot varum leads to prolonged pronation through midstance and into terminal stance to allow for the inside of the forefoot to contact the ground surface. During the beginning of midstance and into terminal stance of a normal running gait, the subtalar joint re-supinates to change the foot into an effective rigid lever for toe-off. However, a runner’s gait with forefoot varum may exhibit prolonged pronation throughout midstance causing the subtalar joint to rapidly re-supinate and create a rigid lever for toe-off. Prolonged pronation into midstance followed by an attempt of the subtalar joint to re-supinate causes a bowstring effect on the Achilles tendon (Figure 12). The bowstring effect places an increased eccentric load on the medial side of the Achilles tendon, predisposing it to injury (5, 15, 23, 24).
 The subtalar joint in a runner with a flat inside arch (pes planus) tends to overpronate, causing an increased eccentric strain on the Achilles tendon. The subtalar joint in a runner with a rigid high inside arch (pes cavus) has limited pronation. Limited pronation decreases the ability of the foot and ankle to absorb ground forces, leading to transmission of excessive forces through the Achilles tendon and other adjacent structures.
The subtalar joint in a runner with a flat inside arch (pes planus) tends to overpronate, causing an increased eccentric strain on the Achilles tendon. The subtalar joint in a runner with a rigid high inside arch (pes cavus) has limited pronation. Limited pronation decreases the ability of the foot and ankle to absorb ground forces, leading to transmission of excessive forces through the Achilles tendon and other adjacent structures.
Runners in their 30s and 40s have an increased risk of developing Achilles tendon injury because the collagen (supportive subunits of muscles, tendons, and ligaments) of the triceps surae degrades with age (16). Without adequate time to rest and heal between bouts of exercise the tricep surae of these athletes are predisposed to injury. To prevent injury older athletes should train on softer surfaces and cross-train with exercises such as cycling, swimming, cross country skiing, rollerblading, and use of a quality elliptical machine.
Factors predisposing an athlete to developing Achilles tendon injuries include tight gastrocnemius and soleus musculature, overpronation and increased velocity of pronation from initial contact through the beginning of midstance, prolonged pronation during midstance, age-related degenerative processes of the Achilles tendon, and training programs that do not allow for adaptation of the Achilles tendon. Initial training programs that incorporate too many uphills or downhills, high intensity interval training, and excessive mileage, lead to injury because the Achilles tendon is not allowed to adapt.
GRADES OF TENDON INJURIES AND PHASES OF TISSUE REPAIR AND TREATMENT
There are five grades of tendon injuries:
Grade 1 – Pain does not occur during normal activity, but generalized pain is felt in the Achilles tendon about 1 to 3 hours after sport-specific training has ended. Tenderness in the Achilles tendon usually resolves within 24 hours without intervention.
Grade 2 – Minimal pain is present in the Achilles tendon towards the end of the sport-specific training session, but performance is not affected. Appropriate treatment may be necessary to prevent a Grade 3 injury.
Grade 3 – Pain is present in the Achilles tendon at the onset of training, and interferes with the speed and duration of a training session. Treatment and training modification are necessary to prevent a grade 3 injury from progressing to a grade 4 injury.
Grade 4 – Pain in the Achilles tendon restricts training and is also noticeable during activities of daily living; the athlete can no longer continue sport-specific training. Low impact training, such as swimming and biking, can be implemented for cardiovascular fitness and aggressive musculoskeletal therapy can decrease the severity of the injury. The goal of therapy is to restore structural integrity of the tissues allowing for the athlete to return to pain-free sport-specific training.
Grade 5 – Pain in the Achilles tendon interferes with training as well as activities of daily living. The Achilles tendon becomes deformed and there is a loss of function of the triceps surae (5). Aggressive therapy is required and surgery may be necessary.
Conservative therapy is usually successful for treatment of Achilles tendon injury. A thorough history and examination will help find the cause of the Achilles tendon injury. Was the injury caused by improper training techniques, age related degenerative changes, a tight tricep surae or biomechanical dysfunction of the rear or forefoot? Initial goals of therapy are to reduce swelling and inflammation of the tendon and paratendon to alleviate acute tendon injury or chronic flare-ups so the patient can perform activities of daily living with less pain. Pain-free modified training can then be implemented to improve strength and flexibility of the triceps surae, as well as cardiovascular fitness. The end goal is to return the athlete to pain free running. However, even if the pain dissipates, the athlete should be made aware that it takes time for the Achilles tendon to regain full strength and function. With fewer blood vessels then muscles, tendons have a limited oxygen and nutrient supply. Faced with this shortage, tendons take a longer time to heal than muscles.
There are three phases of tissue repair: the reactive phase, the regenerative phase, and the remodeling phase. The reactive phase is the initial inflammatory response to microtrauma. Vasodilation of the blood vessels surrounding the injured tendon or muscle occurs, causing swelling, pain, and loss of function. To limit the immobilizing effects of the reactive phase, RICE (rest, ice, compression, and elevation) should be applied to the injured region. During the regenerative phase dead cells are cleared out, tiny blood vessels are restructured to help supply oxygen to the damaged tissue, and collagen is laid down for repair. The reparative collagen is initially weak, but with time its strength improves. After 7-14 days, damaged muscle regains approximately 50% of its strength; tendons may take a longer time to regain their strength. During the remodeling phase, the reparative collagen matures. After completing a proper medical treatment program and complying with a home strength-training and flexibility routine, the athlete may regain 100% strength. The remodeling phase can take up to six months for muscle repair and even longer for tendon repair, depending on the severity of the injury (11, 17, 18).
Appropriate treatment of a grade 1 or a grade 2 Achilles tendon injury consists of:
1. Manual adjustments to the ankle and foot to free up joint motion (25).
2. Deep tissue procedures, such as Graston Technique and Active Release Technique, to break up scar tissue in the affected tendon or paratenon and restore soft tissue motion and glide (19).
3. Ultrasound and electric muscle stimulation are useful modalities to restore normal muscle tone, help in the healing process, and decrease pain (17, 20).
 4. Inflammation reduction by icing the Achilles tendon for 20 minutes on, 1 hour off, repeating throughout the day, and use of NSAIDs (non-steroidal anti-inflammatory drugs) per primary doctor recommendation. Iontophoresis with dexamethasone is also a useful modality to decrease inflammation.
4. Inflammation reduction by icing the Achilles tendon for 20 minutes on, 1 hour off, repeating throughout the day, and use of NSAIDs (non-steroidal anti-inflammatory drugs) per primary doctor recommendation. Iontophoresis with dexamethasone is also a useful modality to decrease inflammation.
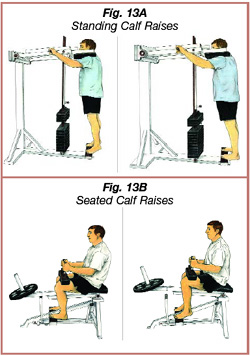
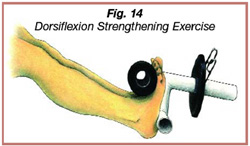
5. A strength training program for the gastrocnemius and soleus musculature, including standing and seated calf raises (Figure 13A and 13B). Studies have indicated that emphasizing eccentric strength training of the triceps surae has been beneficial in treatment and prevention of future Achilles tendon injuries (26, 27). Dorsiflexion strengthening exercises should also be implemented to increase the strength of the tibialis anterior and extensor musculature (Figure 14). Strengthening exercises should progress appropriately with no or little discomfort.
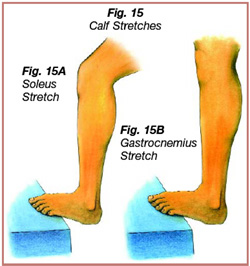
6. Use of a step or slant board to stretch the triceps surae (Figure 15A and 15B). A stretching and strengthening routine for the lower extremities, using a resistive band, can be implemented to improve strength of the dorsiflexors and evertors and flexibility of the hamstring and calf musculature.
 7. A recommendation to replace running sneakers after 250-400 miles of use, at which point the shoe loses 40% of its shock absorption abilities.
7. A recommendation to replace running sneakers after 250-400 miles of use, at which point the shoe loses 40% of its shock absorption abilities.
8. The possible recommendation of appropriate arch supports. A runner with a flat inside arch, pes planus, will usually overpronate, placing an increased strain on the Achilles tendon. A good sneaker with a firm heal counter and an inside arch support will aid in correcting overpronation and help in preventing Achilles tendon injury. If the Achilles tendon injury does not resolve with sneaker adjustment, a semi-rigid orthotic with no more than 5/8” medial arch support is useful. A temporary 1/8” heel lift can also be added to the orthotic to limit dorsiflexion of the foot; this takes pressure off of the injured Achilles tendon. A runner with a high inside arch has limited pronation and poor shock absorption. The high arch runner should get a sneaker with good cushioning; if necessary a semi-rigid orthotic or cushioned liner can be added (3, 4, 8, 13, 28).
 9. A night splint that maintains the ankle and foot in slight dorsiflexion can help to alleviate morning stiffness in the Achilles tendon (23). For more advanced cases of Achilles tendon injury a walking splint can alleviate stress on the slowly healing tendon.
9. A night splint that maintains the ankle and foot in slight dorsiflexion can help to alleviate morning stiffness in the Achilles tendon (23). For more advanced cases of Achilles tendon injury a walking splint can alleviate stress on the slowly healing tendon.
10. Recommendations for appropriate training limits. For marathon runners, an initial training base of four miles at 65%-75% maximum heart rate. A gradual progressive training schedule should follow. A proper warm-up, consisting of a slow jog, increases the blood supply to the muscles and tendons, making them more efficient in absorbing loads. Hill training should be added gradually to a training route because uphill running increases the eccentric load on the Achilles tendon.
Early therapy and intervention are important to prevent a grade 3 tendon injury from progressing to a grade 4 or a grade 5 tendon injury. In the early stages of a grade 3 tendon injury, one week of modified activity is recommended, along with treatments similar to those administered for grade 1 and grade 2 injuries. Modified activity with swimming, running in the pool, bicycling, or using a quality elliptical machine maintains aerobic fitness and allows the triceps surae to heal properly before the athlete resumes full training. Treatment of a more advanced grade 3 or grade 4 tendon injury involves a longer bout of modified activity, rest from the offending activity, and a slower progression of weight training and stretching (3, 4, 18).
Chronic Achilles tendon injuries may not always resolve with conservative therapy. Initially, microscopic tears in the Achilles tendon or paratendon repair naturally with Type III collagen. Type III collagen is immature, disorganized scar tissue that temporarily binds the damaged tendon fibers. Type III collagen is later replaced by Type I collagen, mature scar tissue that has a similar parallel arrangement of fibers as the normal tendon tissue. With time and a properly progressed rehabilitation program the Type I collagen scar regains the tensile strength of the normal tendon tissue. However, sometimes the type III collagen is not always replaced by type I collagen in the later stages of healing. The immature scar tissue remains a chronically inflamed and weakened structure that may be palpated as a tender nodule, usually located on the medial side of the Achilles tendon. The degenerative scar tissue may be resistant to conservative care, and attempting to train on the injured tendon may cause further injury. An athlete who wants to return to running without pain may need to consider surgery. Magnetic Resonance Imaging has been shown to be extremely sensitive to pathological changes in the Achilles tendon and may be a useful tool for the surgeon in discovering degenerative tissue that needs debridement. Surgery usually involves excision of the degenerative intratendinous lesion, followed by rehabilitation. In cases of chronic paratenonitis “brisement” – distension of the paratenon-tendon-interface may help to resolve paratenonitis (23, 29, 30, 31).
CONCLUSION
Athletes participating in sports involving repetitive jumping and running are predisposed to developing Achilles tendon injury. Achilles tendon injuries can be reduced by following a properly progressed training program that allows for adaptation of the Achilles tendon to adapt to increased eccentric loads. Certain biomechanical dysfunction, such as, rearfoot varus, forefoot varus, pes cavus, tight and weak triceps surae, and age-related degenerative changes, also predispose an athlete to Achilles tendon injury. To prevent injury athletes with these dysfunctions should incorporate proper sneaker wear – if necessary semi-rigid orthotics – as well as lower body flexibility, strength and cross training. Achilles tendon injuries can usually be treated successfully with a conservative rehabilitation program that includes modified training and incorporates eccentric strength training of the triceps surae. The athlete must be made aware that it takes time for the Achilles tendon to heal even with rehabilitation. After the Achilles tendon regains function and becomes pain free, the athlete should implement an appropriate training program to prevent re-injury. Sometimes Achilles tendon injuries are resistant to conservative therapy. In such cases surgery and proper rehabilitation may be necessary to remove the degenerative tissue from the tendon or paratendon to allow for proper healing and restoration of strength and function.
REFERENCES
1. Scioli MW. Achilles Tendinitis. Orthopedic Clinics of North America. 1994; 25(1): 177-182.
2. Scott SH, Winter DA. Internal forces at chronic running injury sites. Medicine and Science in Sports and Exercise. 1990; 22(3): 357-369.
3 James SL, Bates BT, Osternig LR. Injuries to runners. The American Journal of Sports Medicine. 1978; 6(2): 40-50.
4. Clement DB, Taunton JE, Smart GW. Achilles tendonitis and peritendinitis: Etiology and treatment. The American Journal of Sports Medicine. 1984; 12(3): 179-184.
5. Sundqvist H, Forsskahl B, Kvist M. A promising novel therapy for Achilles peritendinitis. International Journal of Sports Medicine. 1987; (8): 298-303.
6. Donatelli RA. The Biomechanics of the Foot and Ankle. F.A. Davis Company. 1996; (2nd edition).
7. Backman C, Friden J, Widmark A. Blood flow in chronic Achilles tendinosis. Acta Orthop Scand. 1991; 62(4): 386-387.
8. Schepsis AA, Leach RE. Surgical management of Achilles tendonitis. The American Journal of Sports Medicine. 1987; 15(4): 308-315.
9. Kalebo P, Allenmark C, Peterson L, Sward L. Diagnostic value of ultrasonography in partial ruptures of the Achilles tendon. The American Journal of Sports Medicine. 1992; 20(4): 378-381.
10. Martti KH, Lehto MU, Laszlo J, Markku J, Helmer KT. An immunohistologic study of fibrinectin and fibrinogen. The American Journal of Sports Medicine. 1988; 16(6): 616-623.
11. Banks AS, Downey MS, Martin DE, Miller SJ. Foot and Ankle Surgery. Lipincott Williams and Wilkins. 2002; 2 (3rd edition).
12. Norkin CC, Levangie PK. Joint Structure and Function: A Comprehensive Analysis. 1992; 2nd edition: 448-458.
13. Michaud TC. Foot Orthosis and Other Forms of Conservative Foot Care. 1997.
14. Rodgers MM. Dynamic Biomechanics of the Normal Foot and Ankle During Walking and Running. Physical Therapy. 1988; 12(68): 1822-1829.
15. Smart GW, Tanton JE, Clement DB. Achilles Tendon Disorders in Runners. Medicine and Science in Sports and Exercise. 1980; 4: 231-243.
16. Strocchi R, Depasquale V, Guizzardi S, et al. Human Achilles tendon: morphological and morphometric variations as a function of age. Foot Ankle. 1991; 12: 100-104.
17. Reid D. Sports Injury Assessment and Rehabilitation. Churchill Livingston International. 1992.
18. Leadbetter WB. Cell Matrix Response in Tendon Injury. Clinics in Sports Medicine. 1992; 11(3): 533-579.
19. Kvist M, Jarvinen M. Clinical Histochemical and Biomechanical Features in Repair of Muscle and Tendon Injuries. International Journal of Sports Medicine. 1982; (3): 12-14.
20. Gum SL, Reddy GK, Stehno-Bittel L, et al. Combined ultrasound, electric stimulation, and laser promote collagen synthesis with moderate changes in tendon biomechanics. American Journal of Physical Medicine and Rehabilitation. 1997; 76: 288-296.
21. Hamill J, Bates BT, Holt KG. Timing of lower extremity joint actions during treadmill running. Medicine and Science in Sports and Exercise. 1991; 807-813.
22. Astrom M, Westlin N. Blood Flow in Chronic Achilles Tendinopathy. Clinical Orthopaedics. 1994; (308): 166-172.
23. Schepsis AA, Jones H, Haas LA. Achilles Tendon Disorders in Athletes. The American Journal of Sports Medicine. 2002; 30(2): 287-305.
24. Tiberno D. Pathomechanics of Structural Foot Deformities. Physical Therapy. 1988; 68(12): 1840-1849.
25. Menetrey J, Fritschy D. Subtalar Subluxation in Ballet Dancers. The American Journal of Sports Medicine. 1999; 27(2): 143-149.
26. Shalabi A, Wilberg MK, Svennson L, Aspelin P, Movin T. Eccentric Training of the Gastrocnemius- Soleus Complex in Chronic Achilles Tendinopathy Results in Decreased Tendon Volume and Intratendinous Signal as Evaluated by MRI. The American Journal of Sports Medicine. 2004; 32(5): 1286-1296.
27. Fahlstrom M, Lorentzon R, Alfredson H. Painful Conditions in the Achilles Tendon Region in Elite Badminton Players. The American Journal of Sports Medicine. 2002; 20 (1): 51-54.
28. Gross ML, Davlin L, Evanski PM. Effectiveness of Orthotic Shoe Inserts in the Long-Distance Runner. 1991; 19: 409-412.
29. Maffulli N, Ewen SB.W., Waterston SW, Reaper J, Barrass V. Tenocytes from Ruptured and Tendinopathic Achilles Tendons Produce Greater Quantities of Type III Collagen than Tenocytes from Normal Achilles Tendons. The American Journal of Sports Medicine. 2000; 28(4): 499-505.
30. Paavola M, Kannus P, Paakkala T, Pasanen M, Jarvinen M. Long Term Prognosis of Patients with Achilles Tendinopathy. The American Journal of Sports Medicine. 2000; 28(5): 634-642.
31. Maffulli N, Testa V, Capasso G, Sullo A. Calcific Insertional Achilles Tendinopathy. The American Journal of Sports Medicine. 2004; 32(1): 174-182.
Special thanks to Audrey Mahoney for creating the illustrations.

